Neglected tropical diseases (NTDs) are a group of preventable and treatable parasitic, viral, bacterial, fungal, and non-communicable diseases that affect more than one billion people globally. Of the 20 NTDs in the world, 5 account for the largest burden of disease and can be targeted with safe and effective medicine: Trachoma; Lymphatic filariasis (Also known as elephantiasis); Onchocerciasis (Also known as river blindness); Schistosomiasis (Also known as snail fever); Soil-transmitted helminth infections (hookworm, roundworm, whipworm).
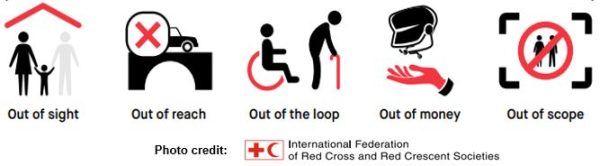
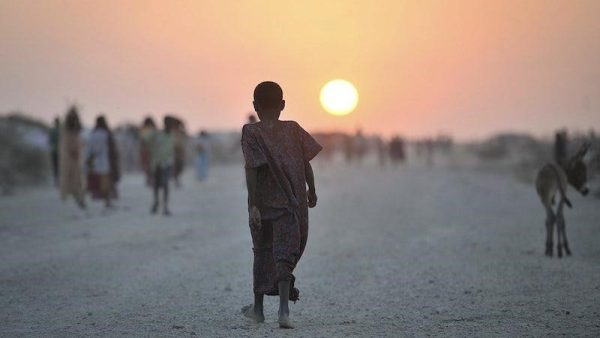
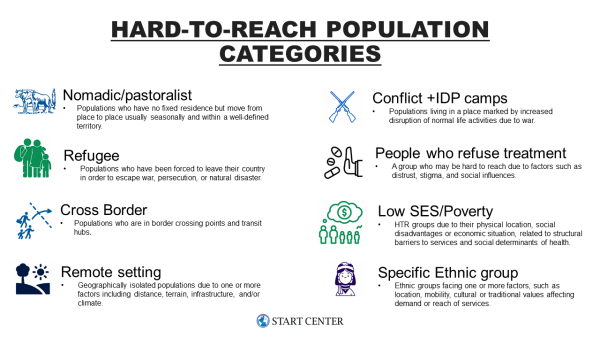
Systemic noncompliance is the biggest threat to elimination efforts and is characterized by weak programs and lack of access to certain areas and communities. To reach elimination targets, it is critical to identify hard-to-reach populations (HTRPs), assess barriers hindering the uptake of NTD programs, and explore optimal channels for expanding coverage. HTRPs are often sub-groups of the general population that have higher exposure to infection and/or are missed by health services and interventions. HTRPs must be reached to (1) Reduce Transmission, (2) Reach Elimination, (3) Achieve Equity.
The Neglected Tropical Diseases team at the Bill & Melinda Gates Foundation commissioned a project with the START Center to conduct a literature review and extract established and potential strategies that can be used to engage and tailor NTD interventions for HTRPs. First, using the BEST framework developed by the Neglected Tropical Disease NGO Network, the START team identified and classified HTRPs into eight categories. The BEST acronym stands for interventions targeting Behavior, Environment, Social Inclusion, and Treatment. This framework provides a standardized approach for a set of comprehensive NTD interventions as well as a clear structure through which NTD investment can be made and results effectively measured by stakeholders.
 Following, the START team completed a literature review using both a broad search string and individual search strings for each NTD category, included 6 pieces of grey literature from INGO/NGO documents, and held 8 key informant interviews.
Following, the START team completed a literature review using both a broad search string and individual search strings for each NTD category, included 6 pieces of grey literature from INGO/NGO documents, and held 8 key informant interviews.
Implementing programs in HRTPs for NTDs is complex and faces barriers as variable as the population categories themselves. Notably, the tools and strategies that have helped NTD programs make huge strides for most of the population may not be the same tools for the "last mile efforts" as they are not sufficiently adapted to HTRPs. The ten strategies below have had success in reaching HTRPs as part of NTD programming, when introduced independently or in combination. Established strategies such as community driven mass drug administration (MDA), micro planning, social mobilization, and integrated care proved most successful from local to international levels. Novel strategies such as GIS mapping, livestock collars, and "test & treat" interventions had some evidence of success, primarily at the local level.
- One Health Approaches: Particularly useful for pastoralist communities, the joint delivery of human + animal health services (e.g. child + animal vaccination)
- Livestock Collaring: Allows for tracking of livestock and/or pastoralist community movement using apps.
- Mapping Hotspots: Use of GIS or fine-scale mapping to map high endemicity hotspots.
- Micro Planning: A bottom-up approach to the organization, planning, and management of all NTD intervention elements at a district level.
- Engage + Test: Identification of individuals who were missed during a campaign (e.g. due to work, travel, etc.) to offer treatment.
- Test + Treat: Identification of individuals who previously refused treatment to offer testing + treatment.
- Community Driven MDA: Engaging local community members to deliver mass drug administration can be more cost-efficient and increase uptake due to established trust.
- Social Mobilization: Engaging/identifying HTRPs through community networks and interpersonal communication.
- Integrated Care: Joint delivery of NTD + other health services (e.g. MDA + vaccinations).
- Enhanced Data Collection: Particularly useful in displaced settings, the use of interoperable data collection devices such as ODK to gather coverage data post MDA.





